Katharine S. Walter is an infectious disease epidemiologist based in Salt Lake City.
ST. GEORGE, Utah — At the peripheries of one of the fastest-growing metropolitan areas in the U.S., the drought-stricken Mojave Desert is being consumed, one heaping scoop of red earth at a time.
The rich habitat of the threatened Mojave desert tortoise is being excavated to make space for new developments, including luxury resorts and so-called master-planned communities with golf courses and water features. Meanwhile, a rapidly warming climate has increased the intensity of Utah’s droughts and the dust storms that accompany them. Dust from construction sites blows into homes, covering counters and floors; some residents develop mysterious coughs and pneumonia.
Here, like in much of the arid American West, Valley fever is on the rise. The fungal infection, which is caused by inhaling spores found in soil and dust, is little discussed and often misdiagnosed, but it is a frequent cause of pneumonia and occasionally results in infection that spreads beyond the lungs, and sometimes, into the brain. In some cases, Valley fever can be deadly.
Construction workers and farm workers whose work brings them close to dust, are on the front lines of this epidemic, with little means to protect themselves. Yet we have only a vague understanding of where the fungus is now, much less how the rapid transformation of southwestern landscapes by both development and climate change will change who is at risk of infection. Unfamiliar diseases are appearing in new places, forcing patients to chase diagnoses and proper medical care.
Searching For A Diagnosis
In July 2018, Kathy Allen returned to her home in southwestern Utah from a trip to Europe with a horrible cough. By the end of the month, she was coughing so much that she went to a health clinic. She was told that she had bronchitis, and then pneumonia, and was prescribed amoxicillin, an antibiotic, ineffective for fungal infections, and a nebulizer to help clear her airways. But her cough continued, and her lungs felt “tight and heavy.”
In October, a pulmonologist found spots on her lungs and prescribed her more antibiotics. In December, imaging showed “hot active cancer” in her lymph nodes. In January 2019, she recalls a thoracic surgeon in northern Utah told her: “You have cancer. This needs to be resolved.” He drew a picture of the spots on her lungs and told her he would go into her lungs and cut those spots out.
Just two weeks before her lung surgery, Allen spoke with a close friend, a doctor, who recently also had lung surgery. She warned Allen that her surgery scars “felt like a burning knife, in her back, every day” and suggested Allen seek a second opinion, Allen later recalled. Allen called the Huntsman Cancer Institute at the University of Utah, where she remembers being asked by the woman on the line: “Wouldn’t you much rather know where the cancer is coming from and know how to treat it before you have surgery? Let’s get you scheduled.”
Four days later, a pulmonologist ran a battery of tests and conducted a bronchoscopy — a procedure that enables doctors to examine airways in the lungs using a small scope. When she came to, Allen learned that she didn’t have cancer. She was thrilled. Instead, she learned that she had tested positive for the emerging fungal disease known as Valley fever.



The Transformation Of St. George
Five years before she got sick, Allen moved to Washington City, Utah, a small town on the outskirts of St. George. Allen spent lots of time outside, taking frequent neighborhood walks that passed by construction sites. “The whole hill was being developed. The dust was heavy in my home, located just below where all the construction was. I was cleaning dust every day off of counters and floors,” she told me.
Allen became friends with a woman named Diane, who also endured an excruciating search for the cause of her symptoms before finally being diagnosed with Valley fever. Diane insisted on anonymity out of fear of legal reprisals. A relatively recent arrival to the area, Diane moved from Salt Lake City to St. George in the summer of 2020 for the milder weather.
“We didn’t want to shovel snow anymore. And my folks lived down here,” Diane told me. She too talked about the dust. “They’re building a brand-new home right next to us in the red dirt, been doing that for a year,” Diane told me. “When the wind blows, yeah, it creates dust in my house.”
“Dust from construction sites blows into homes, covering counters and floors; meanwhile, some residents develop mysterious coughs and pneumonia.”
A few months after we spoke on Zoom, Diane invited me to her home so she could show me the dust plumes herself. I’d arrived in Utah in September 2022 for an epidemiology position at the University of Utah and had begun to study Valley fever. During graduate school, I studied Lyme disease — another zoonotic disease, transmitted between animals and humans, that was also dramatically increasing in incidence due to environmental changes — in this case, mostly in New England and the Midwest.
As Diane pointed out open construction sites — possible sources of her infection — on a neighborhood drive, I was reminded of conversations I’d had with locals while doing field research on Lyme disease on the East Coast. Again and again, I was told that New England summers had not always been the season of tick bites and Lyme disease that they are now. The risk and fear of Lyme disease — like Valley fever — was relatively recent.
St. George is the largest city in Washington County, a county that has the highest rate of Valley fever infection in the state. Known as a “gateway to Zion National Park,” the city is famous for its red rocks, proximity to national parks, and stunning sunsets. St. George is also the hottest city in Utah and has broken July heat records two years in a row.
This July, the average high temperature was 107.9 degrees, six degrees hotter than the average July high from 1991 to 2020. Despite the heat, the county’s population has quadrupled since 1990, increasing from about 49,000 people to more than 200,000. Fueling the increase has been a flurry of luxury housing developments—many advertising themselves as sustainable communities — golf courses and a new water park.
Many come here for dirt biking and ATV riding, generating major soil disturbances that have been linked to Valley fever outbreaks. Many, like Allen and Diane, come to retire, making the area around St. George also older than much of Utah, and more likely to be on immunosuppressing drugs, and generally more vulnerable to infections, due to a phenomenon known as immunosenescence.
This made St. George the perfect place to study how development and climate change collectively impact the risk of infection. About a year after I arrived in Utah, I drove south on I-15 with a dust scientist, in an SUV packed with N95s and soup ladles repurposed for soil collection. We were closely followed by a pair of mammalogists in a truck stocked with a few hundred rodent traps. Somewhere below the area’s glowing cliffs, temple steeples and hillsides scattered with rocks, including one with the letter “D” for Dixie State University (renamed Utah Tech University in 2022), we expected to find the Valley fever fungus.



Searching For Fungi
Shortly after 8 a.m. on a Sunday last October, Katrina Derieg picked up a narrow shoebox-sized metal box, a Sherman rodent trap used by biologists to capture small mammals alive, and peeked inside. “Deer mouse!”— the morning’s third. A hapless white-tailed antelope squirrel had wandered into a trap the night before, just minutes after Derieg, the vertebrate collections manager at the Natural History Museum of Utah, had set them. Derieg had supplied food — peanut butter and oatmeal — and toilet paper, so the squirrel could create a nest and stay warm through the high desert’s cool night.
We were following one of Derieg’s trap lines — 40 traps set along a transect on a mesa above Santa Clara, Utah, a few miles southwest of Diane’s house. Each time Derieg spotted a closed trap, she would call out the species: “Kangaroo rat — cutie! I knew we’d find a kangaroo rat here.” As we walked through the twiggy black brush and taller creosote bushes, many still with star-shaped yellow flowers, the morning light hit the red cliffs before us.
The dogma has long been that the fungus that causes Valley fever is soil-dwelling and that humans and other mammals are so-called accidental hosts, dead ends from the fungus’ perspective. In the soil, it grows as mycelia — long, invisible threads that can break off into single-celled infectious spores, get churned into dust clouds, and inhaled by humans and other animals.
The two largest known outbreaks of Valley fever were associated with historic dust storms: the 1977 Tempest from Tehachapi, a dust storm in California’s Central Valley; and the plumes of dust caused by landslides from the 1994 Northridge earthquake in the San Fernando Valley near Los Angeles.
“St. George [was] the perfect place to study how development and climate change collectively impact the risk of infection.”
The fungus seems to be restricted to hot, dry regions of the American southwest, Mexico, and pockets of Central and South America. Morgan Gorris, an earth systems scientist at Los Alamos National Laboratory, has projected that increasing temperatures and changes in rainfall will more than double the area of the U.S. endemic to the infection and that the number of Valley fever cases will increase by 50% by the end of the century. Not only is the range of Coccidioides expected to increase under climate change, but increasing weather extremes that come with climate change are predicted to increase the risk of disease in places where it is already endemic.
A study led by Jennifer Head and Justin Remais, epidemiologists at the University of Michigan and the University of California, Berkeley, found support for what is known as the “grow and blow” hypothesis in patterns of Valley fever cases in California. Periods of intense rainfall fuel mycelial growth in the soil. When this is followed by increasingly hot, dry and dusty summers, conditions are ideal for wind-blown dispersion of fungal spores that lead to human exposures.
But Coccidioides is also considered a “meat-eating fungus” to some, like Bridget Barker, a biologist at Northern Arizona University, and mycologist John Taylor at the University of California, Berkeley. They argue that the fungus lives in the lungs of small mammals, securely encased in granulomas, small cavities surrounded by immune cells, much like those that develop when someone has tuberculosis. Barker and Taylor hypothesize that when rodents die, their carcasses are abundant sources of food for mycelia to grow, release spores, and infect other small mammals as they burrow through the now-infected soils. Work in Barker’s laboratory has found that rodent burrows are more likely to be infected with Coccidioides than nearby soils. Taylor’s group, in turn, has found that the Coccidioides genome has evolved a capacity for so-called meat-eating.
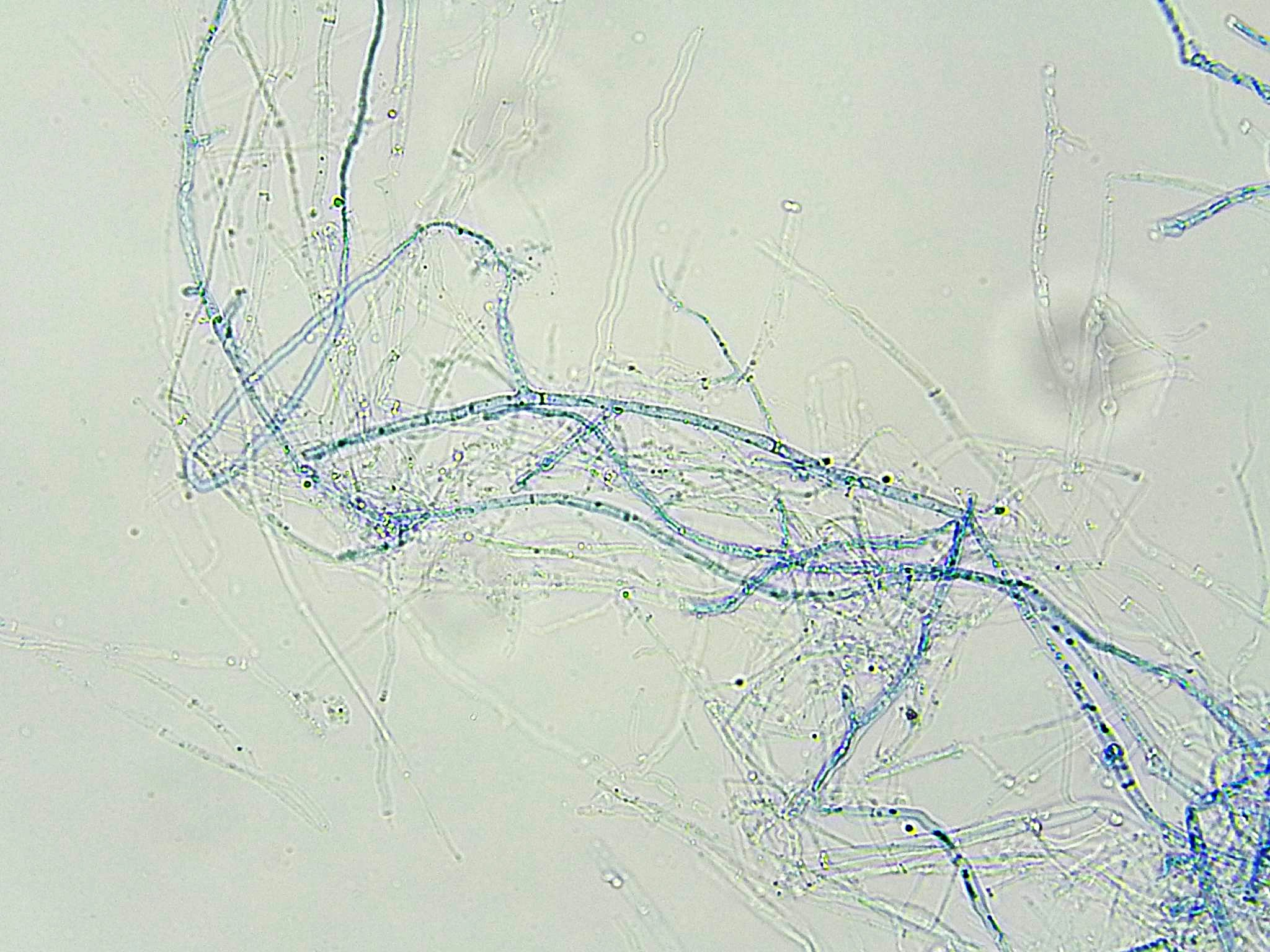
Their work suggests that small mammals may play an important role in understanding where the fungus is now, how it moves, and where it will be in the coming decades. Zoonotic diseases — like Valley fever, Lyme disease and Covid-19 — are among the diseases most impacted by global change. Animals quickly shift ranges to survive changes in temperature and rainfall, and to escape destruction of their preferred habitats, carrying infections with them.
But for now, it is unclear which mammals are the important reservoirs for the Valley fever fungus, and how the increasingly hot and dusty St. George climate and the loss of their habitat would affect them. So we went looking for rodents and their burrows to try to answer these questions.
Redrawing Mycelium Maps
No vaccines yet exist for Valley fever, though a few are in development. In the absence of a vaccine, the U.S. Centers for Disease Control and Prevention (CDC) advises “people who are at higher risk for severe Valley fever should try to avoid breathing in large amounts of dust if they’re in these [endemic] areas.”
This is a difficult recommendation for anyone to follow — and nearly impossible for anyone unhoused or whose work puts them in close contact with dust. Avoiding infection is all the more difficult since the current CDC risk map of Valley fever is wildly unrepresentative and dated, largely based on more than 70-year-old studies run by the U.S. government.
Valley fever became a military priority during World War II when men from across the country were brought to the southwest for training and thousands fell sick. To address this, the U.S. Public Health Service conducted skin testing for 89,000 men who reported to the Naval Training Center in San Diego between 1949 and 1951, as well as female nursing students and undergraduates at a few colleges in the Midwest and Northeast.
Even short visits to endemic areas could result in infection. You could roll down your window at an unlucky spot on a drive down Highway 1 in the west, the story goes, and wind up sick. To be more specific in their map, researchers included results only from people who had lived in one county their entire lives and were between 17 and 21 years old. With no justification, their study excluded anyone who wasn’t white, making it impossible to draw broader conclusions from their study about who was at risk of infection.
“Periods of intense rainfall fuel mycelial growth in the soil. When this is followed by increasingly hot, dry and dusty summers, conditions are ideal for … human exposures.”
Not only is the U.S. an average of 4 degrees Fahrenheit warmer than when the skin testing study was completed, and western landscapes are in many places unrecognizable, but outbreaks outside of the CDC’s map indicate that we don’t yet have a clear idea of the fungus’ range.
Between June 29 and July 3, 2001, a group of 10 volunteers and archaeologists working at Dinosaur National Monument in northeastern Utah and northwestern Colorado rushed to the local ER — all were having trouble breathing, most were coughing and feverish, some had developed rashes on their necks and torsos. The group — six students, two leaders and two National Park Service archaeologists — had been working at a site called Swelter Shelter, a sandstone overhang that holds Fremont Culture pictographs, petroglyphs and artifacts dating as far back as 7000 to 6000 B.C.
Swelter Shelter faces south, making it a sandstone heat trap. On June 19, 10 workers sifted dirt through screens for artifacts, generating “considerable dust” and ultimately fell ill with Valley fever, according to the CDC report. Eight were hospitalized and treated with antifungal drugs. Disturbingly, the monument is 200 miles north of what was considered the endemic range of the fungus at the time.
CDC epidemiologists also contacted the archaeologists who’d worked at Swelter Shelter in the ‘60s. Five described having had fever, cough and chest pain symptoms consistent with Valley fever, including one archaeologist who was hospitalized for 10 days after digs in the ‘60s.
In 2010, another cluster of Valley fever cases appeared far north of what was considered its range, in eastern Washington State, which has a climate similar to the southwest. At first, it was unclear whether the individuals had been infected outside of Washington — all three had traveled to other endemic places in prior years. But each reported likely exposures: a 12-year-old who biked and played in the dirt in a nearby desert canyon, a 15-year-old who fell sick after an ATV crash and a 58-year-old who worked as a construction excavator.
That year, and again in 2014, CDC epidemiologists tested soil from where the 12 and 15-year-olds were likely infected. Many of the soil samples were positive, and fungal genome sequences from both locations almost perfectly matched the fungal genome from a culture taken from the twelve-year-old.
One of the consequences of a biased and outdated Valley fever risk map is that people may not know of the risk it poses, and healthcare providers — like those Allen and Diane first encountered — may not be looking for it. Valley fever is a largely invisible epidemic — the CDC estimates that tens of thousands of cases go unreported each year. Many of these unreported cases may be among asymptomatic people or those whose symptoms resolved quickly, but others would benefit from treatment.
A recent study found higher rates of Valley fever mortality in Utah than in other states. This is probably not due to a particularly virulent fungal strain in Utah, but instead due to long delays in proper diagnosis and treatment because of relatively low levels of awareness in Utah compared to Arizona or California’s Central Valley.
The Desert’s Ecological Richness
The word desert is an Old French word that means “wilderness, wasteland” or “destruction, ruin” and originates, in turn, from the Latin word desertum, or “thing abandoned.” Ads for new developments suggest that golf courses and hotels are springing up across St. George and the surrounding desert from some sort of void.
But this image disregards the desert’s exquisite ecological fullness and variation, and the rich human history in the region, including that of the Ancestral Puebloans and the Southern Paiutes, who occupied what is now St. George for millennia before Mormon settlers arrived.
Eric Rickart is among those well acquainted with desert diversity. Rickart, curator of vertebrates at the Natural History Museum of Utah, has spent his career studying rodents across the mountainous regions of the American West and in the Philippines.
When I met with Rickart in July, he wore a black T-shirt that said, “There’s nothing like a cold, dead rat!” with a grim picture of an Isarog striped shrew-rat, Chrotomys gonzalesi, a species he identified and named. C. gonzalesi, I learned, is also the mascot for Dead Rat Brewing, Rickart’s homebrew.
Once on a research trip, a medical mycologist in our group asked Rickart about his favorite mammal and he began to describe Chrotomys whiteheadi, the Luzon striped rat that lives in the Philippine mountains and survives mostly on earthworms. He interrupted himself: “My favorite mammal is my wife.”
“Outbreaks outside of the CDC’s map indicate that we don’t yet have a clear idea of the fungus’ range.”
Derieg and Rickart first showed our team rodent burrows, which soon began to pop out of the muted desert landscape like Easter eggs — deliberate holes of various sizes beneath the black brush and creosote bushes, and under sandstone slabs. The sand was a canvas for their activity: looping tail drags and delicate footprints leading to burrow entrances.
While Derieg and Rickart followed traplines, I worked with Kevin Perry, an atmospheric scientist at the University of Utah, to carefully angle small soup ladles into burrows and scoop soil into plastic conical tubes. Perry’s recent research has focused on dust, and he has documented the dust plumes emanating from the Great Salt Lake’s widening exposed playa.
Our first trapping trip was “wildly successful,” a 68% trap success, Derieg reported, leaving Derieg and Rickart with the work of conducting necropsies on 108 mammals — mostly canyon mice, long-tailed pocket mice, and cactus mice. “You can do that in a desert in a good year. These animals are easy to trap,” Rickart said. Derieg told me to temper my expectations for future field trips: a 10% trap success was considered good.
A few hundred yards downslope from Derieg’s trap line, development was expanding into the canyon mouse habitat. A billboard with a QR code advertised the new lots and a machine sprayed water onto a large pile of recently excavated dirt to suppress the rising dust.

Preventing Spillover
In the heady discussions about how to prevent the next pandemic, Raina Plowright, a bat biologist and disease ecologist at Cornell University, has been making the case for conservation. Pathogens are plentiful in ecosystems around the world, but pandemics — often arising from spillovers of infection from wild animals — are rare, she wrote in a research paper published earlier this year.
Pandemics require a disastrous alignment of conditions that most often occur on fragmented landscapes where zoonotic reservoirs are pushed out of natural habitats and put in close contact with people lacking prior exposures or immunity.
The combined impact of habitat destruction and climate change force zoonotic disease reservoirs across the world to shift their ranges, leading to “viral sharing” among species that have been historically isolated — and potentially leading to spillover of these new viruses to humans.
Billions of dollars have been spent on biomedical responses to outbreaks and pandemics. Masks, vaccines and antiviral drugs have saved innumerable lives. But unequal access to these technologies magnifies the glaring inequities in global health. At the height of the Covid-19 pandemic, for example, pharmaceutical companies refused to loosen patents on vaccine formulas, making vaccine doses too expensive for much of the world. The resulting “vaccine apartheid,” as Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization (WHO), calls it, caused countless preventable deaths.
What if we instead were to prevent spillover from occurring in the first place? Plowright argues that protecting and restoring the habitat of zoonotic reservoir species would minimize human interactions with those reservoirs, preventing pathogens from jumping into humans. This could be more equitable than the costly biomedical responses we have developed.
The Valley fever fungus likely won’t cause the next pandemic. Yet conserving the ecosystems where fungal reservoirs reside — including the native desert vegetation that keeps mycelia in the ground and limits dust from blowing — and taking every available action to avoid the worst possible future climate scenarios, may similarly be our most effective and cheapest defenses against the next pandemic.
“This is something Indigenous people have known for a long time — not to make scars on the land,” Rose Ann Abrahamson, a Lemhi Shoshone historian and translator, told me.
Dry Creek Reservoir
On a spring field trip, our sampling team drove southeast along Old Highway 91, leaving the Shivwits Band of Paiutes reservation — a fragment of the more than 30 million acres Southern Paiutes inhabited for millennia —and entering Ivins. Here, undisturbed desert shrub habitat gave way to a perplexing number of ongoing construction sites. Waves of dust visibly rose from open red fields of earth and heaps of soil. At one site, four yellow excavators were parked in a row, their massive arms poised in parallel above the soil, like masochistic ballerinas frozen in place at the start of some sick ballet.
“What if we instead were to prevent spillover [of wild animal infections] from occurring in the first place?”
Locals worried that Ivins, an artsy community of about 10,000, nine miles northwest of St. George, was about to get a lot dustier. The area’s ballooning population and expanding golf scene require water, scarce in an arid desert experiencing its 24th year of megadrought. The Washington County Water Conservancy District had proposed a reservoir. The idea was to store treated wastewater, so-called reuse water, locally for outdoor irrigation, making more water available for imminent development projects already approved by the city.
The tracks of a Mojave desert tortoise — listed as threatened under the federal Endangered Species Act — were spotted at the first proposed reservoir site, according to a manager at the Washington County Water Conservancy District, stalling construction plans there. Heated community debate now focused on an alternate proposed reservoir site, Dry Wash — an undeveloped open space located between Ivins and the Shivwits Band of the Paiutes reservation.
Early one morning this past May, my research assistant and I pulled up behind Ginamarie Foglia’s white Land Rover at Dry Wash. In front of a barbed wire fence surrounding the property, someone had put up a small sign: “View the proposed Natural Park Site? Or Reservoir Site?” and printed maps of the alternatives. Reservoirs rise and fall with the seasons, a dynamic that will be further intensified by climate change.
Foglia, an infectious disease clinician in Ivins, and others, including Utah Physicians for a Healthy Environment, worried that when water levels were low in the summer months, 47 acres of reservoir bed would be exposed, blowing dust and potentially, harmful chemicals and fungal spores, directly into neighboring homes. Here, it was not just climate change, but developers’ hasty responses to climate change-driven drought, that could dangerously amplify disease.
Wooden stakes and hot pink flagging tape marked the reservoir’s planned perimeter. We walked down a hillside into what could soon be underwater, crossing a dried-up creek, its exposed rocks thick with salt. Somehow, fat tadpoles survived in a shady pool. Empty was not a word that came to mind, as we walked by blooming desert marigolds and fragrant sagebrush, kneeling at plentiful rodent burrows to collect soil samples, scouring the ground for tortoise tracks.
Watching Dust Plumes
After visits to urgent care, an emergency room, and a course of antibiotics, Diane asked her family doctor in St. George if she might have Valley fever. Her doctor told her it was unlikely and sent her to a rheumatologist for a lung biopsy and cancer test. There, she insisted on a Valley fever test too. After 10 excruciating days, her results came back positive for Valley fever. “You’re the first one I’ve ever seen that has it,” she recalled the rheumatologist telling her.
Diane, whose living room has views of the sprawling construction, blames the ongoing growth of St. George for her diagnosis. “They’re building homes there by the lava rocks … building out by the airport. We’re talking huge developments that will bring hundreds of thousands of people,” she said. “I worry for people.”
More projects designed to draw increasing crowds are on the horizon and are backed by powerful political supporters. The Salt Lake Tribune reported that developers are considering building a sports arena in the area that could accommodate up to 12,500 people. Republican state Sen. Jerry Stevenson said that he might sponsor a bill to provide state funding for it as a public infrastructure project.
A previous analysis from the Tribune reported that Stevenson, along with more than one-third of Utah’s state legislature profits from development. Meanwhile, Washington County is fighting to build a four-lane highway through Red Cliffs National Conservation Area north of St. George — a critical habitat for Mojave desert tortoises and several native Virgin River fish — to move tourists and residents across the city more quickly.
“The City is well on its way to accomplishing its tourism goals,” the 2024 Ivins City General Plan states.
But Diane is less satisfied.
“They’re so proud of all this growth,” she told me, “and it’s killing us.”